По поводу расшифровки Pulmonary Function Test
Pulmonary Function Tests: Categories & Calculations
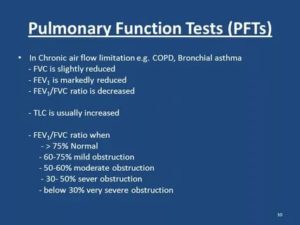
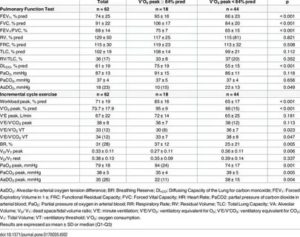
Image: Doing a spirometry, by Jmarchn. License: CC BY-SA 3.0
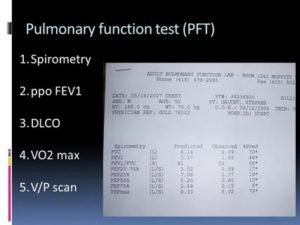
PFT (pulmonary function tests) can measure lung mechanics (spirometry and lung volumes) or the gas exchange/diffusion function of the respiratory system.
Spirometry: FVC and FEV1
- Measures volume of air exhaled as a function of time
- Restrictive lung disease has a reduced volume, i.e. a low FVC
- Obstructive lung disease has a reduced flow, i.e. a low FEV1
Lung volumes: TLC, RV
- The addition of 2 or more volumes comprises a capacity
- Nitrogen washout and helium dilution technique
- Body plethysmography is the standard for measuring lung volumes
Image: Body box with male subject enclosed, by Finchbook01. License: CC BY-SA 3.0
Gas Exchange: DLCO, AaDO2
- Ability to transport gas from alveoli to blood
- Estimates surface area available for gas exchange
- Depends on hemoglobin (Hb) and cardiac output
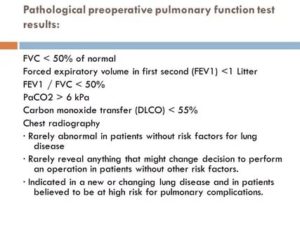
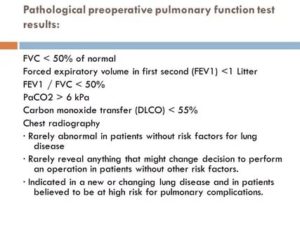
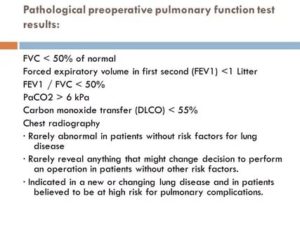
Indication of PFT
Pulmonary function tests (PFT) are mainly diagnostic/prognostic.
- Diagnostic: screening of at-risk patients, such as age > 70 years, obese; evaluation of chronic cough; follow-up for patients with chronic lung disease
- Prognostic: before lung surgery, to evaluate response to drugs, and to assess the degree of disability
Contraindications of PFT
Recent eye surgery, abdominal aneurysms, hemoptysis, pneumothorax, and recent myocardial infarction.
Volumes
Tidal volume (TV or VT): volume of air inhaled or exhaled during regular respiration at rest; normal value: 500 ml
Inspiratory reserve volume (IRV): volume of air that can be maximally inhaled above and after a normal tidal inspiration; normal value: 3,000 ml
Expiratory reserve volume (ERV): volume of air that can be maximally exhaled after a normal tidal expiration; normal value: 1,500 ml
Residual volume (RV): the amount of air that remains in the lungs after maximal forced exhalation; cannot be measured directly by spirometry but is indirectly calculated as RV = FRC – ERV; normal value: 20–25mL/kg or 1,200 mL.
Capacities (sum of 2 or more volumes)
Total lung capacity (TLC): volume of air present in lungs after maximum deep inspiration; the sum of all volumes: TLC = IRV + TV + ERV + RV; normal value: 5,000–6,000 ml
Vital capacity (VC): maximum volume of air exhaled after a maximum deep inspiration: VC = IRV + TV + ERV or VC = TLC – RV; normal value: 4,500–5,000 ml
Inspiratory capacity (IC): maximum volume of air inspired after a normal tidal expiration: IC = TV + IRV; normal value: 2,400–3,600 ml
Expiratory capacity (EC): maximum volume of air expired after normal tidal inspiration: EC = TV+ ERV; normal value: 1,800–2,300 ml
Functional residual capacity (FRC): volume of air remaining in the lungs after normal tidal expiration: FRC = ERV + RV.
FRC is an important component that maintains a continuous exchange of oxygen and carbon dioxide at the alveolar-capillary membrane.
Collapse or atelectasis of the lungs leads to a reduction in FRC, causing hypoxemia and hypercarbia. The normal value is 2,500 ml.
Image: Functional residual capacity
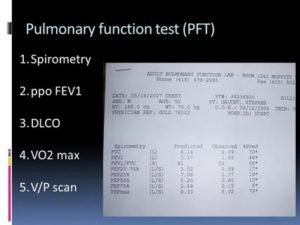
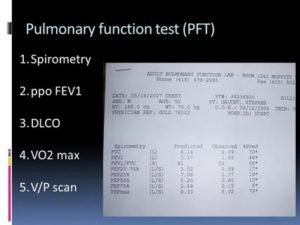
Spirometry
Image: Doing a spirometry, by Jmarchn. License: CC BY-SA 3.0
Spirometry is the most frequently used measure of pulmonary function. It measures the volume of air inhaled or exhaled by the patient as a function of time. The patient is asked to take a deep inspiration and then to forcefully expel air, as quickly and as long as possible. The results of the test include:
- Forced vital capacity (FVC): maximum volume of air forcefully exhaled after a maximal inspiration. This is usually reduced in restrictive lung disease; however, an obstructive lung disease with significant hyperinflation can also cause reduced FVC.
- FEV1: volume of air exhaled during the initial second of the FVC maneuver.
- The ratio of FEV1/FVC: Normal value is > 75%. The value is decreased in obstructive lung disease. Values < 50% suggests a severe obstruction.
- FEF 25–75% (forced mid-expiratory flow): maximum flow rate during mid-expiratory part of the FVC maneuver. Expressed in L/min, it represents the status of small airways. Normal value is 300 L/min.
- PEFR (peak expiratory flow rate): Maximal flow rate during the FVC maneuver occurs in the initial 0.1 seconds. It gives a crude estimate of larger airway function. Normal value is 400–700 L/min.
Important: Spirometry does not measure volumes such as FRC, TC, and RV.
Two patterns of results are identified: obstructive and restrictive diseases.
In obstructive diseases, a reduction in flow is predominant, leading to low FEV1; however, FVC may be normal or low. Hence, the FEV1/FVC ratio is usually < 0.7.
Reversibility: An increase in FEV1 by 12–15% on repeat spirometry after administration of a bronchodilator (salbutamol) is characteristic of asthma.
[attention type=green][attention type=red][attention type=yellow]In restrictive diseases, a reduction in lung volume is predominant, which leads to low FVC; however, FEV1 may be normal or low. Hence, FEV1/FVC ratio is > 0.7 (and may be > 1.0).
[/attention][/attention][/attention]
This needs confirmation, as RV cannot be measured by spirometry (low RV is the hallmark of restrictive lung disease).
Loop spirometry
Image: Loop spirometry
Flow volume loops are formed when a patient performs the spirometry maneuver, and a graph is plotted with the volume on the x-axis and the flow on the y-axis. The expiratory limb is usually represented as positive.
The initial one-third of the expiratory flow is effort dependant; the latter part is effort independent; hence the shape.
The inspiratory limb is entirely effort dependent, and the curve is smooth (useful for identifying the phase of respiration if not labeled).
In the obstructive pattern of the flow-volume loop, there is a decrease in the height of the y-axis, which represents decreased air flow. The volume remains normal or high (hyper-inflation). In the restrictive pattern, there is predominantly reduced volume, which is more prominent than the decrease in flow.
Image: Loop spirometry
Limitation of spirometry
Spirometry cannot measure RV or TLC. It is important to differentiate the cause of decreased VC in a patient suffering from chronic obstructive pulmonary disease (COPD). In COPD, VC can be reduced in two scenarios:
- The patient has a superimposed restrictive lung disease.
- The patient has significant hyper-inflation.
These can be differentiated using lung volume measurement. The former will have a reduced TLC, while hyper-inflation will show increased TLC. Hence, a confirmation by lung volume studies is necessary.
Detection of upper airway obstruction–other spirometry patterns
Image: Detection of upper airway obstruction
- Fixed airway obstruction: constant limitation of flow during inspiration and expiration; for example: stricture, goiter, or stenosis
- Variable extrathoracic obstruction: Reduction in flow is greater during inspiration (airways tend to collapse during inspiration due to negative transmural pressure). Positive pressure in airway during expiration decreases obstruction. For example: vocal cord palsy, obstructive sleep apnea
- Variable intrathoracic obstruction: Reduction inflow is greater during expiration (high pleural pressure decreases airway diameter). During inspiration, lower pleural pressure around the airway tends to decrease obstruction. For example: tracheomalacia, tumor of bronchus
Gas dilution technique
N2 washout: Patient breathes 100% oxygen, so that all nitrogen in the lungs is washed out. The difference in nitrogen volume at initial exhaled concentration and final concentration gives the value of FRC.
He dilution: Patient breathes from a reservoir containing a known volume of gas with a trace of helium. The inhaled helium gets diluted in the gas present in lungs.
The concentration of helium in the exhaled gas is expressed as a percentage, giving the lung volume.
For example, if the patient breathes 50 mL of helium, and its concentration in the exhaled gas is 1%, the volume of the lung is 5 L.
Plethysmography
The patient sits inside an airtight body box with a known volume. The patient pants with an open glottis against a closed shutter. The increase in chest volume reduces the relative box volume and increases the box pressure. Measurements are done during expiration, and hence FRC is measured. The principal behind plethysmography is Boyle’s law (P x V = K).
Important: Lung volumes, such as RV, FRC, and TLC, cannot be measured by spirometry.
Applications of volume testing
- Measures RV, FRC, and TLC (which spirometry cannot measure)
- Spirometry only measures FVC, which can be misleading when used alone.
- Reduced RV, FRC, and TLC is seen in restrictive diseases interstitial lung disease, sarcoidosis, or fibrosis.
- Increased RV, FRC, and TLC is seen in obstructive lung diseases asthma, COPD, and cystic fibrosis.
DLCO (Diffusion capacity of Carbon Monoxide)
The patient inspires a diluted mixture of CO and is told to hold their breath for 10 seconds. The amount of CO taken up is then measured by infrared analysis.
DLCO = CO (ml/min/mm Hg) ÷ PACO – PcCO
CO is the ideal gas for this study, as it has a very high affinity for Hb and very low plasma/lung concentration. It demonstrates the ability of the lung to transport inhaled gas from the alveoli to the blood. Normal value is 20–30 ml/min/mm Hg.
DLCO values depend on three factors:
- Thickness and permeability of alveolar-capillary membrane (increased in pulmonary bleeding, interstitial lung disease)
- Hemoglobin concentration
- Cardiac output
Factors altering DLCO
| Decrease DLCO (< 80%) | Increase DLCO (> 120%) |
| Anemia | Polycythemia |
| Emphysema | Exercise |
| Fibrosis | Congestive heart failure |
Alveolar to arterial oxygen tension gradient (AaDO2)
- Detects the difference between alveolar oxygen (PaO2) and arterial oxygen tension (PaO2)
- Needs arterial blood gas analysis for PaO2
- Normal values are below 10 mm Hg, and values above 100 mm Hg indicate significant impairment in gas exchange.
Cardiopulmonary reserve/exercise testing
- The stair-climbing test and 6-minute walk test measure changes in SaO2/SpO2, HR, and oxygen utilization (VaO2).
- These tests analyze the individual’s ability to cope with increased metabolic demands during exercise.
- They give a clear picture of the functional improvement of a patient during follow-up.
Summary
| Parameter | Obstructive lung disease | Restrictive lung disease |
| TLC | High/normal | Very low |
| VC or FVC | Low/normal | Very low |
| RV | High | Low |
| FRC | High | Low |
| FEV1 | Very Low | Normal/low |
| FEV1/FVC | Low | Normal/high |
| Peak flow | Low | Low |
| Examples | COPD, asthma | Interstitial lung disease, fibrosis |
Источник: https://www.lecturio.com/magazine/pulmonary-function-tests-pft/
Pulmonary Function Test: Purpose, Procedure & Risks
Pulmonary function tests (PFTs) are a group of tests that measure how well your lungs work. This includes how well you’re able to breathe and how effective your lungs are able to bring oxygen to the rest of your body.
Your doctor may order these tests:
- if you’re having symptoms of lung problems
- if you’re regularly exposed to certain substances in the environment or workplace
- to monitor the course of chronic lung disease, such as asthma or chronic obstructive pulmonary disease (COPD)
- to assess how well your lungs are working before you have surgery
PFTs are also known as lung function tests.
Your doctor will order these tests to determine how your lungs are working. If you already have a condition that’s affecting your lungs, your doctor may order this test to see if the condition is progressing or how it’s responding to treatment.
PFTs can help diagnose:
- asthma
- allergies
- chronic bronchitis
- respiratory infections
- lung fibrosis
- bronchiectasis, a condition in which the airways in the lungs stretch and widen
- COPD, which used to be called emphysema
- asbestosis, a condition caused by exposure to asbestos
- sarcoidosis, an inflammation of your lungs, liver, lymph nodes, eyes, skin, or other tissues
- scleroderma, a disease that affects your connective tissue
- pulmonary tumor
- lung cancer
- weaknesses of the chest wall muscles
If you’re on medications that open your airways, such as those used for asthma or chronic bronchitis, your doctor may ask you to stop taking them before the test.
If it isn’t clear whether or not you should take your medication, make sure to ask your doctor. Pain medications may also affect the results of the test.
You should tell your doctor about any over-the-counter and prescription pain medications you’re taking.
[attention type=yellow][attention type=green][attention type=red]It’s important that you don’t eat a large meal before testing. A full stomach can prevent your lungs from inhaling fully.
[/attention][/attention][/attention]
You should also avoid food and drinks that contain caffeine, such as chocolate, coffee, and tea, before your test. Caffeine can cause your airways to be more open which could affect the results of your test.
You should also avoid smoking at least an hour before the test, as well as strenuous exercise before the test.
Be sure to wear loose-fitting clothing to the test. Tighter clothing may restrict your breathing. You should also avoid wearing jewelry that might affect your breathing. If you wear dentures, wear them to the test to ensure that your mouth can fit tightly around the mouthpiece used for the test.
If you have had recent eye, chest, or abdominal surgery or a recent heart attack, you will ly need to delay the test until you have fully recovered.
Your PFTs may include spirometry, which measures the amount of air you breathe in and out. For this test, you’ll sit in front of a machine and be fitted with a mouthpiece.
It’s important that the mouthpiece fits snugly so that all the air you breathe goes into the machine. You’ll also wear a nose clip to keep you from breathing air out through your nose.
The respiratory technologist will explain how to breathe for the test.
You may then breathe normally. Your doctor will ask you to breathe in and out as deeply or as quickly as you can for several seconds. They may also ask you to breathe in a medication that opens your airways. You’ll then breathe into the machine again to see if the medication affected your lung function.
Plethysmography test
A plethysmography test measures the volume of gas in your lungs, known as lung volume. For this test, you’ll sit or stand in a small booth and breathe into a mouthpiece. Your doctor can learn about your lung volume by measuring the pressure in the booth.
Diffusion capacity test
This test evaluates how well the small air sacks inside the lungs, called alveoli, work. For this part of a pulmonary function test, you will be asked to breathe in certain gases such as oxygen, helium, or carbon dioxide.
You may also breathe in a “tracer gas” for one breath. The machine can detect when you breathe out this gas. This tests how well your lungs are able to transfer oxygen and carbon dioxide to and from your bloodstream.
A PFT can cause problems if:
- you’ve recently had a heart attack
- you’ve recently had eye surgery
- you’ve recently had chest surgery
- you’ve recently had abdominal surgery
- you have a severe respiratory infection
- you have unstable heart disease
PFTs are usually safe for most people. However, because the test may require you to breathe in and out quickly, you may feel dizzy and there’s a risk that you may faint. If you feel lightheaded, tell your doctor. If you have asthma, the test may cause you to have an asthma attack. In very rare cases, PFTs may cause a collapsed lung.
Источник: https://www.healthline.com/health/pulmonary-function-tests
Pulmonary Function Tests
Linkedin Pinterest
Pulmonary function tests (PFTs) are noninvasive tests that show how wellthe lungs are working. The tests measure lung volume, capacity, rates offlow, and gas exchange. This information can help your healthcare providerdiagnose and decide the treatment of certain lung disorders.
There are 2 types of disorders that cause problems with air moving in and the lungs:
- Obstructive. This is when air has trouble flowing the lungs due to airway resistance. This causes a decreased flow of air.
- Restrictive. This is when the lung tissue and/or chest muscles can’t expand enough. This creates problems with air flow, mostly due to lower lung volumes.
PFT can be done with 2 methods. These 2 methods may be used together andperform different tests, depending on the information that your healthcareprovider is looking for:
- Spirometry. A spirometer is a device with a mouthpiece hooked up to a small electronic machine.
- Plethysmography. You sit or stand inside an air-tight box that looks a short, square telephone booth to do the tests.
PFT measures:
- Tidal volume (VT). This is the amount of air inhaled or exhaled during normal breathing.
- Minute volume (MV). This is the total amount of air exhaled per minute.
- Vital capacity (VC). This is the total volume of air that can be exhaled after inhaling as much as you can.
- Functional residual capacity (FRC). This is the amount of air left in lungs after exhaling normally.
- Residual volume. This is the amount of air left in the lungs after exhaling as much as you can.
- Total lung capacity. This is the total volume of the lungs when filled with as much air as possible.
- Forced vital capacity (FVC). This is the amount of air exhaled forcefully and quickly after inhaling as much as you can.
- Forced expiratory volume (FEV). This is the amount of air expired during the first, second, and third seconds of the FVC test.
- Forced expiratory flow (FEF). This is the average rate of flow during the middle half of the FVC test.
- Peak expiratory flow rate (PEFR). This is the fastest rate that you can force air your lungs.
Normal values for PFTs vary from person to person. The amount of airinhaled and exhaled in your test results are compared to the average forsomeone of the same age, height, sex, and race. Results are also comparedto any of your previous test results. If you have abnormal PFT measurementsor if your results have changed, you may need other tests.
Why might I need pulmonary function tests?
There are many different reasons why pulmonary function tests (PFTs) may bedone. They are sometimes done in healthy people as part of a routinephysical.
They are also routinely done in certain types of workenvironments to ensure employee health (such as graphite factories and coalmines).
Or you may have PFTs if your healthcare provider needs help todiagnose you with a health problem such as:
- Allergies
- Respiratory infections
- Trouble breathing from injury to the chest or a recent surgery
- Chronic lung conditions, such as asthma, bronchiectasis, emphysema, or chronic bronchitis
- Asbestosis, a lung disease caused by inhaling asbestos fibers
- Restrictive airway problems from scoliosis, tumors, or inflammation or scarring of the lungs
- Sarcoidosis, a disease that causes lumps of inflammatory cells around organs, such as the liver, lungs, and spleen
- Scleroderma, a disease that causes thickening and hardening of connective tissue
PFTs may be used to check lung function before surgery or other proceduresin patients who have lung or heart problems, who are smokers, or who haveother health conditions. Another use of PFTs is to assess treatment forasthma, emphysema, and other chronic lung problems. Your healthcareprovider may also have other reasons to advise PFTs.
What are the risks of pulmonary function tests?
Because pulmonary function testing is not an invasive procedure, it is safeand quick for most people. But the person must be able to follow clear,simple directions.
All procedures have some risks. The risks of this procedure may include:
- Dizziness during the tests
- Feeling short of breath
- Coughing
- Asthma attack brought on by deep inhalation
In some cases, a person shouldn’t have PFTs. Reasons for this can include:
- Recent eye surgery, because of increased pressure inside the eyes during the procedure
- Recent belly or chest surgery
- Chest pain, recent heart attack, or an unstable heart condition
- A bulging blood vessel (aneurysm) in the chest, belly, or brain
- Active tuberculosis (TB) or respiratory infection, such as a cold or the flu
Your risks may vary depending on your general health and other factors. Askyour healthcare provider which risks apply most to you. Talk with him orher about any concerns you have.
Certain things can make PFTs less accurate. These include:
- The degree of patient cooperation and effort
- Use of medicines that open the airways (bronchodilators)
- Use of pain medicines
- Pregnancy
- Stomach bloating that affects the ability to take deep breaths
- Extreme tiredness or other conditions that affect a person’s ability to do the tests (such as a head cold)
How do I get ready for pulmonary function tests?
Your healthcare provider will explain the procedure to you. Ask him or herany questions you have. You may be asked to sign a consent form that givespermission to do the procedure. Read the form carefully. Ask questions ifanything is not clear.
Tell your healthcare provider if you take any medicines. This includesprescriptions, over-the-counter medicines, vitamins, and herbalsupplements.
Make sure to:
- Stop taking certain medicines before the procedure, if instructed by your healthcare provider
- Stop smoking before the test, if instructed by your healthcare provider. Ask your provider how many hours before the test you should stop smoking.
- Not eat a heavy meal before the test, if instructed by your healthcare provider
- Follow any other instructions your healthcare provider gives you
Your height and weight will be recorded before the test. This is done sothat your results can be accurately calculated.
What happens during pulmonary function tests?
You may have your procedure as an outpatient. This means you go home thesame day. Or it may be done as part of a longer stay in the hospital. Theway the procedure is done may vary. It depends on your condition and yourhealthcare provider's methods. In most cases, the procedure will followthis process:
You’ll be asked to loosen tight clothing, jewelry, or other things that may cause a problem with the procedure.
If you wear dentures, you will need to wear them during the procedure.
You’ll need to empty your bladder before the procedure.
You’ll sit in a chair. A soft clip will be put on your nose. This is so all of your breathing is done through your mouth, not your nose.
You’ll be given a sterile mouthpiece that is attached to a spirometer.
You’ll form a tight seal over the mouthpiece with your mouth. You’ll be instructed to inhale and exhale in different ways.
You will be watched carefully during the procedure for dizziness, trouble breathing, or other problems.
You may be given a bronchodilator after certain tests. The tests will then be repeated several minutes later, after the bronchodilator has taken effect.
What happens after pulmonary function tests?
If you have a history of lung or breathing problems, you may be tired afterthe tests. You will be given a chance to rest afterwards. Your healthcareprovider will talk with you about your test results.
Источник: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pulmonary-function-tests
Pulmonary Function Tests: Categories & Calculations
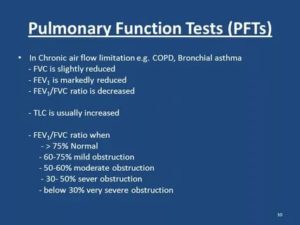
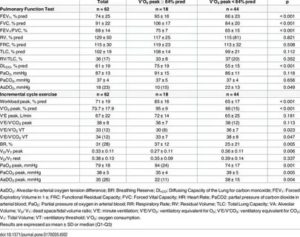
Image: Doing a spirometry, by Jmarchn. License: CC BY-SA 3.0
PFT (pulmonary function tests) can measure lung mechanics (spirometry and lung volumes) or the gas exchange/diffusion function of the respiratory system.
Spirometry: FVC and FEV1
- Measures volume of air exhaled as a function of time
- Restrictive lung disease has a reduced volume, i.e. a low FVC
- Obstructive lung disease has a reduced flow, i.e. a low FEV1
Lung volumes: TLC, RV
- The addition of 2 or more volumes comprises a capacity
- Nitrogen washout and helium dilution technique
- Body plethysmography is the standard for measuring lung volumes
Image: Body box with male subject enclosed, by Finchbook01. License: CC BY-SA 3.0
Gas Exchange: DLCO, AaDO2
- Ability to transport gas from alveoli to blood
- Estimates surface area available for gas exchange
- Depends on hemoglobin (Hb) and cardiac output
Indication of PFT
Pulmonary function tests (PFT) are mainly diagnostic/prognostic.
- Diagnostic: screening of at-risk patients, such as age > 70 years, obese; evaluation of chronic cough; follow-up for patients with chronic lung disease
- Prognostic: before lung surgery, to evaluate response to drugs, and to assess the degree of disability
Contraindications of PFT
Recent eye surgery, abdominal aneurysms, hemoptysis, pneumothorax, and recent myocardial infarction.
Volumes
Tidal volume (TV or VT): volume of air inhaled or exhaled during regular respiration at rest; normal value: 500 ml
Inspiratory reserve volume (IRV): volume of air that can be maximally inhaled above and after a normal tidal inspiration; normal value: 3,000 ml
Expiratory reserve volume (ERV): volume of air that can be maximally exhaled after a normal tidal expiration; normal value: 1,500 ml
Residual volume (RV): the amount of air that remains in the lungs after maximal forced exhalation; cannot be measured directly by spirometry but is indirectly calculated as RV = FRC – ERV; normal value: 20–25mL/kg or 1,200 mL.
Capacities (sum of 2 or more volumes)
Total lung capacity (TLC): volume of air present in lungs after maximum deep inspiration; the sum of all volumes: TLC = IRV + TV + ERV + RV; normal value: 5,000–6,000 ml
Vital capacity (VC): maximum volume of air exhaled after a maximum deep inspiration: VC = IRV + TV + ERV or VC = TLC – RV; normal value: 4,500–5,000 ml
Inspiratory capacity (IC): maximum volume of air inspired after a normal tidal expiration: IC = TV + IRV; normal value: 2,400–3,600 ml
Expiratory capacity (EC): maximum volume of air expired after normal tidal inspiration: EC = TV+ ERV; normal value: 1,800–2,300 ml
Functional residual capacity (FRC): volume of air remaining in the lungs after normal tidal expiration: FRC = ERV + RV.
FRC is an important component that maintains a continuous exchange of oxygen and carbon dioxide at the alveolar-capillary membrane.
Collapse or atelectasis of the lungs leads to a reduction in FRC, causing hypoxemia and hypercarbia. The normal value is 2,500 ml.
Image: Functional residual capacity
Spirometry
Image: Doing a spirometry, by Jmarchn. License: CC BY-SA 3.0
Spirometry is the most frequently used measure of pulmonary function. It measures the volume of air inhaled or exhaled by the patient as a function of time. The patient is asked to take a deep inspiration and then to forcefully expel air, as quickly and as long as possible. The results of the test include:
- Forced vital capacity (FVC): maximum volume of air forcefully exhaled after a maximal inspiration. This is usually reduced in restrictive lung disease; however, an obstructive lung disease with significant hyperinflation can also cause reduced FVC.
- FEV1: volume of air exhaled during the initial second of the FVC maneuver.
- The ratio of FEV1/FVC: Normal value is > 75%. The value is decreased in obstructive lung disease. Values < 50% suggests a severe obstruction.
- FEF 25–75% (forced mid-expiratory flow): maximum flow rate during mid-expiratory part of the FVC maneuver. Expressed in L/min, it represents the status of small airways. Normal value is 300 L/min.
- PEFR (peak expiratory flow rate): Maximal flow rate during the FVC maneuver occurs in the initial 0.1 seconds. It gives a crude estimate of larger airway function. Normal value is 400–700 L/min.
Important: Spirometry does not measure volumes such as FRC, TC, and RV.
Two patterns of results are identified: obstructive and restrictive diseases.
In obstructive diseases, a reduction in flow is predominant, leading to low FEV1; however, FVC may be normal or low. Hence, the FEV1/FVC ratio is usually < 0.7.
Reversibility: An increase in FEV1 by 12–15% on repeat spirometry after administration of a bronchodilator (salbutamol) is characteristic of asthma.
[attention type=green][attention type=red][attention type=yellow]In restrictive diseases, a reduction in lung volume is predominant, which leads to low FVC; however, FEV1 may be normal or low. Hence, FEV1/FVC ratio is > 0.7 (and may be > 1.0).
[/attention][/attention][/attention]
This needs confirmation, as RV cannot be measured by spirometry (low RV is the hallmark of restrictive lung disease).
Loop spirometry
Image: Loop spirometry
Flow volume loops are formed when a patient performs the spirometry maneuver, and a graph is plotted with the volume on the x-axis and the flow on the y-axis. The expiratory limb is usually represented as positive.
The initial one-third of the expiratory flow is effort dependant; the latter part is effort independent; hence the shape.
The inspiratory limb is entirely effort dependent, and the curve is smooth (useful for identifying the phase of respiration if not labeled).
In the obstructive pattern of the flow-volume loop, there is a decrease in the height of the y-axis, which represents decreased air flow. The volume remains normal or high (hyper-inflation). In the restrictive pattern, there is predominantly reduced volume, which is more prominent than the decrease in flow.
Image: Loop spirometry
Limitation of spirometry
Spirometry cannot measure RV or TLC. It is important to differentiate the cause of decreased VC in a patient suffering from chronic obstructive pulmonary disease (COPD). In COPD, VC can be reduced in two scenarios:
- The patient has a superimposed restrictive lung disease.
- The patient has significant hyper-inflation.
These can be differentiated using lung volume measurement. The former will have a reduced TLC, while hyper-inflation will show increased TLC. Hence, a confirmation by lung volume studies is necessary.
Detection of upper airway obstruction–other spirometry patterns
Image: Detection of upper airway obstruction
- Fixed airway obstruction: constant limitation of flow during inspiration and expiration; for example: stricture, goiter, or stenosis
- Variable extrathoracic obstruction: Reduction in flow is greater during inspiration (airways tend to collapse during inspiration due to negative transmural pressure). Positive pressure in airway during expiration decreases obstruction. For example: vocal cord palsy, obstructive sleep apnea
- Variable intrathoracic obstruction: Reduction inflow is greater during expiration (high pleural pressure decreases airway diameter). During inspiration, lower pleural pressure around the airway tends to decrease obstruction. For example: tracheomalacia, tumor of bronchus
Gas dilution technique
N2 washout: Patient breathes 100% oxygen, so that all nitrogen in the lungs is washed out. The difference in nitrogen volume at initial exhaled concentration and final concentration gives the value of FRC.
He dilution: Patient breathes from a reservoir containing a known volume of gas with a trace of helium. The inhaled helium gets diluted in the gas present in lungs.
The concentration of helium in the exhaled gas is expressed as a percentage, giving the lung volume.
For example, if the patient breathes 50 mL of helium, and its concentration in the exhaled gas is 1%, the volume of the lung is 5 L.
Plethysmography
The patient sits inside an airtight body box with a known volume. The patient pants with an open glottis against a closed shutter. The increase in chest volume reduces the relative box volume and increases the box pressure. Measurements are done during expiration, and hence FRC is measured. The principal behind plethysmography is Boyle’s law (P x V = K).
Important: Lung volumes, such as RV, FRC, and TLC, cannot be measured by spirometry.
Applications of volume testing
- Measures RV, FRC, and TLC (which spirometry cannot measure)
- Spirometry only measures FVC, which can be misleading when used alone.
- Reduced RV, FRC, and TLC is seen in restrictive diseases interstitial lung disease, sarcoidosis, or fibrosis.
- Increased RV, FRC, and TLC is seen in obstructive lung diseases asthma, COPD, and cystic fibrosis.
DLCO (Diffusion capacity of Carbon Monoxide)
The patient inspires a diluted mixture of CO and is told to hold their breath for 10 seconds. The amount of CO taken up is then measured by infrared analysis.
DLCO = CO (ml/min/mm Hg) ÷ PACO – PcCO
CO is the ideal gas for this study, as it has a very high affinity for Hb and very low plasma/lung concentration. It demonstrates the ability of the lung to transport inhaled gas from the alveoli to the blood. Normal value is 20–30 ml/min/mm Hg.
DLCO values depend on three factors:
- Thickness and permeability of alveolar-capillary membrane (increased in pulmonary bleeding, interstitial lung disease)
- Hemoglobin concentration
- Cardiac output
Factors altering DLCO
| Decrease DLCO (< 80%) | Increase DLCO (> 120%) |
| Anemia | Polycythemia |
| Emphysema | Exercise |
| Fibrosis | Congestive heart failure |
Alveolar to arterial oxygen tension gradient (AaDO2)
- Detects the difference between alveolar oxygen (PaO2) and arterial oxygen tension (PaO2)
- Needs arterial blood gas analysis for PaO2
- Normal values are below 10 mm Hg, and values above 100 mm Hg indicate significant impairment in gas exchange.
Cardiopulmonary reserve/exercise testing
- The stair-climbing test and 6-minute walk test measure changes in SaO2/SpO2, HR, and oxygen utilization (VaO2).
- These tests analyze the individual’s ability to cope with increased metabolic demands during exercise.
- They give a clear picture of the functional improvement of a patient during follow-up.
Summary
| Parameter | Obstructive lung disease | Restrictive lung disease |
| TLC | High/normal | Very low |
| VC or FVC | Low/normal | Very low |
| RV | High | Low |
| FRC | High | Low |
| FEV1 | Very Low | Normal/low |
| FEV1/FVC | Low | Normal/high |
| Peak flow | Low | Low |
| Examples | COPD, asthma | Interstitial lung disease, fibrosis |
Источник: https://www.lecturio.com/magazine/pulmonary-function-tests-pft/
Pulmonary Function Test: Purpose, Procedure & Risks
Pulmonary function tests (PFTs) are a group of tests that measure how well your lungs work. This includes how well you’re able to breathe and how effective your lungs are able to bring oxygen to the rest of your body.
Your doctor may order these tests:
- if you’re having symptoms of lung problems
- if you’re regularly exposed to certain substances in the environment or workplace
- to monitor the course of chronic lung disease, such as asthma or chronic obstructive pulmonary disease (COPD)
- to assess how well your lungs are working before you have surgery
PFTs are also known as lung function tests.
Your doctor will order these tests to determine how your lungs are working. If you already have a condition that’s affecting your lungs, your doctor may order this test to see if the condition is progressing or how it’s responding to treatment.
PFTs can help diagnose:
- asthma
- allergies
- chronic bronchitis
- respiratory infections
- lung fibrosis
- bronchiectasis, a condition in which the airways in the lungs stretch and widen
- COPD, which used to be called emphysema
- asbestosis, a condition caused by exposure to asbestos
- sarcoidosis, an inflammation of your lungs, liver, lymph nodes, eyes, skin, or other tissues
- scleroderma, a disease that affects your connective tissue
- pulmonary tumor
- lung cancer
- weaknesses of the chest wall muscles
If you’re on medications that open your airways, such as those used for asthma or chronic bronchitis, your doctor may ask you to stop taking them before the test.
If it isn’t clear whether or not you should take your medication, make sure to ask your doctor. Pain medications may also affect the results of the test.
You should tell your doctor about any over-the-counter and prescription pain medications you’re taking.
[attention type=yellow][attention type=green][attention type=red]It’s important that you don’t eat a large meal before testing. A full stomach can prevent your lungs from inhaling fully.
[/attention][/attention][/attention]
You should also avoid food and drinks that contain caffeine, such as chocolate, coffee, and tea, before your test. Caffeine can cause your airways to be more open which could affect the results of your test.
You should also avoid smoking at least an hour before the test, as well as strenuous exercise before the test.
Be sure to wear loose-fitting clothing to the test. Tighter clothing may restrict your breathing. You should also avoid wearing jewelry that might affect your breathing. If you wear dentures, wear them to the test to ensure that your mouth can fit tightly around the mouthpiece used for the test.
If you have had recent eye, chest, or abdominal surgery or a recent heart attack, you will ly need to delay the test until you have fully recovered.
Your PFTs may include spirometry, which measures the amount of air you breathe in and out. For this test, you’ll sit in front of a machine and be fitted with a mouthpiece.
It’s important that the mouthpiece fits snugly so that all the air you breathe goes into the machine. You’ll also wear a nose clip to keep you from breathing air out through your nose.
The respiratory technologist will explain how to breathe for the test.
You may then breathe normally. Your doctor will ask you to breathe in and out as deeply or as quickly as you can for several seconds. They may also ask you to breathe in a medication that opens your airways. You’ll then breathe into the machine again to see if the medication affected your lung function.
Plethysmography test
A plethysmography test measures the volume of gas in your lungs, known as lung volume. For this test, you’ll sit or stand in a small booth and breathe into a mouthpiece. Your doctor can learn about your lung volume by measuring the pressure in the booth.
Diffusion capacity test
This test evaluates how well the small air sacks inside the lungs, called alveoli, work. For this part of a pulmonary function test, you will be asked to breathe in certain gases such as oxygen, helium, or carbon dioxide.
You may also breathe in a “tracer gas” for one breath. The machine can detect when you breathe out this gas. This tests how well your lungs are able to transfer oxygen and carbon dioxide to and from your bloodstream.
A PFT can cause problems if:
- you’ve recently had a heart attack
- you’ve recently had eye surgery
- you’ve recently had chest surgery
- you’ve recently had abdominal surgery
- you have a severe respiratory infection
- you have unstable heart disease
PFTs are usually safe for most people. However, because the test may require you to breathe in and out quickly, you may feel dizzy and there’s a risk that you may faint. If you feel lightheaded, tell your doctor. If you have asthma, the test may cause you to have an asthma attack. In very rare cases, PFTs may cause a collapsed lung.
Источник: https://www.healthline.com/health/pulmonary-function-tests
Pulmonary Function Tests
Linkedin Pinterest
Pulmonary function tests (PFTs) are noninvasive tests that show how wellthe lungs are working. The tests measure lung volume, capacity, rates offlow, and gas exchange. This information can help your healthcare providerdiagnose and decide the treatment of certain lung disorders.
There are 2 types of disorders that cause problems with air moving in and the lungs:
- Obstructive. This is when air has trouble flowing the lungs due to airway resistance. This causes a decreased flow of air.
- Restrictive. This is when the lung tissue and/or chest muscles can’t expand enough. This creates problems with air flow, mostly due to lower lung volumes.
PFT can be done with 2 methods. These 2 methods may be used together andperform different tests, depending on the information that your healthcareprovider is looking for:
- Spirometry. A spirometer is a device with a mouthpiece hooked up to a small electronic machine.
- Plethysmography. You sit or stand inside an air-tight box that looks a short, square telephone booth to do the tests.
PFT measures:
- Tidal volume (VT). This is the amount of air inhaled or exhaled during normal breathing.
- Minute volume (MV). This is the total amount of air exhaled per minute.
- Vital capacity (VC). This is the total volume of air that can be exhaled after inhaling as much as you can.
- Functional residual capacity (FRC). This is the amount of air left in lungs after exhaling normally.
- Residual volume. This is the amount of air left in the lungs after exhaling as much as you can.
- Total lung capacity. This is the total volume of the lungs when filled with as much air as possible.
- Forced vital capacity (FVC). This is the amount of air exhaled forcefully and quickly after inhaling as much as you can.
- Forced expiratory volume (FEV). This is the amount of air expired during the first, second, and third seconds of the FVC test.
- Forced expiratory flow (FEF). This is the average rate of flow during the middle half of the FVC test.
- Peak expiratory flow rate (PEFR). This is the fastest rate that you can force air your lungs.
Normal values for PFTs vary from person to person. The amount of airinhaled and exhaled in your test results are compared to the average forsomeone of the same age, height, sex, and race. Results are also comparedto any of your previous test results. If you have abnormal PFT measurementsor if your results have changed, you may need other tests.
Why might I need pulmonary function tests?
There are many different reasons why pulmonary function tests (PFTs) may bedone. They are sometimes done in healthy people as part of a routinephysical.
They are also routinely done in certain types of workenvironments to ensure employee health (such as graphite factories and coalmines).
Or you may have PFTs if your healthcare provider needs help todiagnose you with a health problem such as:
- Allergies
- Respiratory infections
- Trouble breathing from injury to the chest or a recent surgery
- Chronic lung conditions, such as asthma, bronchiectasis, emphysema, or chronic bronchitis
- Asbestosis, a lung disease caused by inhaling asbestos fibers
- Restrictive airway problems from scoliosis, tumors, or inflammation or scarring of the lungs
- Sarcoidosis, a disease that causes lumps of inflammatory cells around organs, such as the liver, lungs, and spleen
- Scleroderma, a disease that causes thickening and hardening of connective tissue
PFTs may be used to check lung function before surgery or other proceduresin patients who have lung or heart problems, who are smokers, or who haveother health conditions. Another use of PFTs is to assess treatment forasthma, emphysema, and other chronic lung problems. Your healthcareprovider may also have other reasons to advise PFTs.
What are the risks of pulmonary function tests?
Because pulmonary function testing is not an invasive procedure, it is safeand quick for most people. But the person must be able to follow clear,simple directions.
All procedures have some risks. The risks of this procedure may include:
- Dizziness during the tests
- Feeling short of breath
- Coughing
- Asthma attack brought on by deep inhalation
In some cases, a person shouldn’t have PFTs. Reasons for this can include:
- Recent eye surgery, because of increased pressure inside the eyes during the procedure
- Recent belly or chest surgery
- Chest pain, recent heart attack, or an unstable heart condition
- A bulging blood vessel (aneurysm) in the chest, belly, or brain
- Active tuberculosis (TB) or respiratory infection, such as a cold or the flu
Your risks may vary depending on your general health and other factors. Askyour healthcare provider which risks apply most to you. Talk with him orher about any concerns you have.
Certain things can make PFTs less accurate. These include:
- The degree of patient cooperation and effort
- Use of medicines that open the airways (bronchodilators)
- Use of pain medicines
- Pregnancy
- Stomach bloating that affects the ability to take deep breaths
- Extreme tiredness or other conditions that affect a person’s ability to do the tests (such as a head cold)
How do I get ready for pulmonary function tests?
Your healthcare provider will explain the procedure to you. Ask him or herany questions you have. You may be asked to sign a consent form that givespermission to do the procedure. Read the form carefully. Ask questions ifanything is not clear.
Tell your healthcare provider if you take any medicines. This includesprescriptions, over-the-counter medicines, vitamins, and herbalsupplements.
Make sure to:
- Stop taking certain medicines before the procedure, if instructed by your healthcare provider
- Stop smoking before the test, if instructed by your healthcare provider. Ask your provider how many hours before the test you should stop smoking.
- Not eat a heavy meal before the test, if instructed by your healthcare provider
- Follow any other instructions your healthcare provider gives you
Your height and weight will be recorded before the test. This is done sothat your results can be accurately calculated.
What happens during pulmonary function tests?
You may have your procedure as an outpatient. This means you go home thesame day. Or it may be done as part of a longer stay in the hospital. Theway the procedure is done may vary. It depends on your condition and yourhealthcare provider's methods. In most cases, the procedure will followthis process:
You’ll be asked to loosen tight clothing, jewelry, or other things that may cause a problem with the procedure.
If you wear dentures, you will need to wear them during the procedure.
You’ll need to empty your bladder before the procedure.
You’ll sit in a chair. A soft clip will be put on your nose. This is so all of your breathing is done through your mouth, not your nose.
You’ll be given a sterile mouthpiece that is attached to a spirometer.
You’ll form a tight seal over the mouthpiece with your mouth. You’ll be instructed to inhale and exhale in different ways.
You will be watched carefully during the procedure for dizziness, trouble breathing, or other problems.
You may be given a bronchodilator after certain tests. The tests will then be repeated several minutes later, after the bronchodilator has taken effect.
What happens after pulmonary function tests?
If you have a history of lung or breathing problems, you may be tired afterthe tests. You will be given a chance to rest afterwards. Your healthcareprovider will talk with you about your test results.
Источник: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pulmonary-function-tests
Pulmonary Function Tests: Categories & Calculations
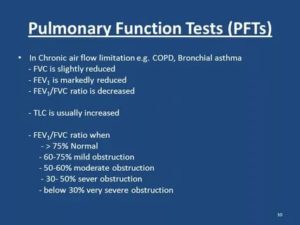
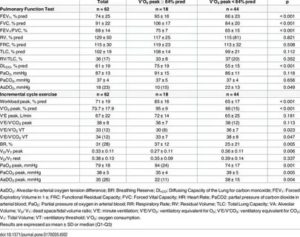
Image: Doing a spirometry, by Jmarchn. License: CC BY-SA 3.0
PFT (pulmonary function tests) can measure lung mechanics (spirometry and lung volumes) or the gas exchange/diffusion function of the respiratory system.
Categories of PFT
There are 3 categories of tests:
Spirometry: FVC and FEV1
- Measures volume of air exhaled as a function of time
- Restrictive lung disease has a reduced volume, i.e. a low FVC
- Obstructive lung disease has a reduced flow, i.e. a low FEV1
Lung volumes: TLC, RV
- The addition of 2 or more volumes comprises a capacity
- Nitrogen washout and helium dilution technique
- Body plethysmography is the standard for measuring lung volumes
Image: Body box with male subject enclosed, by Finchbook01. License: CC BY-SA 3.0
Gas Exchange: DLCO, AaDO2
- Ability to transport gas from alveoli to blood
- Estimates surface area available for gas exchange
- Depends on hemoglobin (Hb) and cardiac output
Indication of PFT
Pulmonary function tests (PFT) are mainly diagnostic/prognostic.
- Diagnostic: screening of at-risk patients, such as age > 70 years, obese; evaluation of chronic cough; follow-up for patients with chronic lung disease
- Prognostic: before lung surgery, to evaluate response to drugs, and to assess the degree of disability
Contraindications of PFT
Recent eye surgery, abdominal aneurysms, hemoptysis, pneumothorax, and recent myocardial infarction.
Lung Volumes and Capacities
Volumes
Tidal volume (TV or VT): volume of air inhaled or exhaled during regular respiration at rest; normal value: 500 ml
Inspiratory reserve volume (IRV): volume of air that can be maximally inhaled above and after a normal tidal inspiration; normal value: 3,000 ml
Expiratory reserve volume (ERV): volume of air that can be maximally exhaled after a normal tidal expiration; normal value: 1,500 ml
Residual volume (RV): the amount of air that remains in the lungs after maximal forced exhalation; cannot be measured directly by spirometry but is indirectly calculated as RV = FRC – ERV; normal value: 20–25mL/kg or 1,200 mL.
Capacities (sum of 2 or more volumes)
Total lung capacity (TLC): volume of air present in lungs after maximum deep inspiration; the sum of all volumes: TLC = IRV + TV + ERV + RV; normal value: 5,000–6,000 ml
Vital capacity (VC): maximum volume of air exhaled after a maximum deep inspiration: VC = IRV + TV + ERV or VC = TLC – RV; normal value: 4,500–5,000 ml
Inspiratory capacity (IC): maximum volume of air inspired after a normal tidal expiration: IC = TV + IRV; normal value: 2,400–3,600 ml
Expiratory capacity (EC): maximum volume of air expired after normal tidal inspiration: EC = TV+ ERV; normal value: 1,800–2,300 ml
Functional residual capacity (FRC): volume of air remaining in the lungs after normal tidal expiration: FRC = ERV + RV.
FRC is an important component that maintains a continuous exchange of oxygen and carbon dioxide at the alveolar-capillary membrane.
Collapse or atelectasis of the lungs leads to a reduction in FRC, causing hypoxemia and hypercarbia. The normal value is 2,500 ml.
Image: Functional residual capacity
Spirometry
Image: Doing a spirometry, by Jmarchn. License: CC BY-SA 3.0
Spirometry is the most frequently used measure of pulmonary function. It measures the volume of air inhaled or exhaled by the patient as a function of time. The patient is asked to take a deep inspiration and then to forcefully expel air, as quickly and as long as possible. The results of the test include:
- Forced vital capacity (FVC): maximum volume of air forcefully exhaled after a maximal inspiration. This is usually reduced in restrictive lung disease; however, an obstructive lung disease with significant hyperinflation can also cause reduced FVC.
- FEV1: volume of air exhaled during the initial second of the FVC maneuver.
- The ratio of FEV1/FVC: Normal value is > 75%. The value is decreased in obstructive lung disease. Values < 50% suggests a severe obstruction.
- FEF 25–75% (forced mid-expiratory flow): maximum flow rate during mid-expiratory part of the FVC maneuver. Expressed in L/min, it represents the status of small airways. Normal value is 300 L/min.
- PEFR (peak expiratory flow rate): Maximal flow rate during the FVC maneuver occurs in the initial 0.1 seconds. It gives a crude estimate of larger airway function. Normal value is 400–700 L/min.
Important: Spirometry does not measure volumes such as FRC, TC, and RV.
Two patterns of results are identified: obstructive and restrictive diseases.
In obstructive diseases, a reduction in flow is predominant, leading to low FEV1; however, FVC may be normal or low. Hence, the FEV1/FVC ratio is usually < 0.7.
Reversibility: An increase in FEV1 by 12–15% on repeat spirometry after administration of a bronchodilator (salbutamol) is characteristic of asthma.
[attention type=green][attention type=red][attention type=yellow]In restrictive diseases, a reduction in lung volume is predominant, which leads to low FVC; however, FEV1 may be normal or low. Hence, FEV1/FVC ratio is > 0.7 (and may be > 1.0).
[/attention][/attention][/attention]
This needs confirmation, as RV cannot be measured by spirometry (low RV is the hallmark of restrictive lung disease).
Loop spirometry
Image: Loop spirometry
Flow volume loops are formed when a patient performs the spirometry maneuver, and a graph is plotted with the volume on the x-axis and the flow on the y-axis. The expiratory limb is usually represented as positive.
The initial one-third of the expiratory flow is effort dependant; the latter part is effort independent; hence the shape.
The inspiratory limb is entirely effort dependent, and the curve is smooth (useful for identifying the phase of respiration if not labeled).
In the obstructive pattern of the flow-volume loop, there is a decrease in the height of the y-axis, which represents decreased air flow. The volume remains normal or high (hyper-inflation). In the restrictive pattern, there is predominantly reduced volume, which is more prominent than the decrease in flow.
Image: Loop spirometry
Limitation of spirometry
Spirometry cannot measure RV or TLC. It is important to differentiate the cause of decreased VC in a patient suffering from chronic obstructive pulmonary disease (COPD). In COPD, VC can be reduced in two scenarios:
- The patient has a superimposed restrictive lung disease.
- The patient has significant hyper-inflation.
These can be differentiated using lung volume measurement. The former will have a reduced TLC, while hyper-inflation will show increased TLC. Hence, a confirmation by lung volume studies is necessary.
Detection of upper airway obstruction–other spirometry patterns
Image: Detection of upper airway obstruction
- Fixed airway obstruction: constant limitation of flow during inspiration and expiration; for example: stricture, goiter, or stenosis
- Variable extrathoracic obstruction: Reduction in flow is greater during inspiration (airways tend to collapse during inspiration due to negative transmural pressure). Positive pressure in airway during expiration decreases obstruction. For example: vocal cord palsy, obstructive sleep apnea
- Variable intrathoracic obstruction: Reduction inflow is greater during expiration (high pleural pressure decreases airway diameter). During inspiration, lower pleural pressure around the airway tends to decrease obstruction. For example: tracheomalacia, tumor of bronchus
Lung Volumes – RV, FRC, TLC
Gas dilution technique
N2 washout: Patient breathes 100% oxygen, so that all nitrogen in the lungs is washed out. The difference in nitrogen volume at initial exhaled concentration and final concentration gives the value of FRC.
He dilution: Patient breathes from a reservoir containing a known volume of gas with a trace of helium. The inhaled helium gets diluted in the gas present in lungs.
The concentration of helium in the exhaled gas is expressed as a percentage, giving the lung volume.
For example, if the patient breathes 50 mL of helium, and its concentration in the exhaled gas is 1%, the volume of the lung is 5 L.
Plethysmography
The patient sits inside an airtight body box with a known volume. The patient pants with an open glottis against a closed shutter. The increase in chest volume reduces the relative box volume and increases the box pressure. Measurements are done during expiration, and hence FRC is measured. The principal behind plethysmography is Boyle’s law (P x V = K).
Important: Lung volumes, such as RV, FRC, and TLC, cannot be measured by spirometry.
Applications of volume testing
- Measures RV, FRC, and TLC (which spirometry cannot measure)
- Spirometry only measures FVC, which can be misleading when used alone.
- Reduced RV, FRC, and TLC is seen in restrictive diseases interstitial lung disease, sarcoidosis, or fibrosis.
- Increased RV, FRC, and TLC is seen in obstructive lung diseases asthma, COPD, and cystic fibrosis.
Gas Exchange Function – DLCO, AaDO2
DLCO (Diffusion capacity of Carbon Monoxide)
The patient inspires a diluted mixture of CO and is told to hold their breath for 10 seconds. The amount of CO taken up is then measured by infrared analysis.
DLCO = CO (ml/min/mm Hg) ÷ PACO – PcCO
CO is the ideal gas for this study, as it has a very high affinity for Hb and very low plasma/lung concentration. It demonstrates the ability of the lung to transport inhaled gas from the alveoli to the blood. Normal value is 20–30 ml/min/mm Hg.
DLCO values depend on three factors:
- Thickness and permeability of alveolar-capillary membrane (increased in pulmonary bleeding, interstitial lung disease)
- Hemoglobin concentration
- Cardiac output
Factors altering DLCO
| Decrease DLCO (< 80%) | Increase DLCO (> 120%) |
| Anemia | Polycythemia |
| Emphysema | Exercise |
| Fibrosis | Congestive heart failure |
Alveolar to arterial oxygen tension gradient (AaDO2)
- Detects the difference between alveolar oxygen (PaO2) and arterial oxygen tension (PaO2)
- Needs arterial blood gas analysis for PaO2
- Normal values are below 10 mm Hg, and values above 100 mm Hg indicate significant impairment in gas exchange.
Cardiopulmonary reserve/exercise testing
- The stair-climbing test and 6-minute walk test measure changes in SaO2/SpO2, HR, and oxygen utilization (VaO2).
- These tests analyze the individual’s ability to cope with increased metabolic demands during exercise.
- They give a clear picture of the functional improvement of a patient during follow-up.
Summary
| Parameter | Obstructive lung disease | Restrictive lung disease |
| TLC | High/normal | Very low |
| VC or FVC | Low/normal | Very low |
| RV | High | Low |
| FRC | High | Low |
| FEV1 | Very Low | Normal/low |
| FEV1/FVC | Low | Normal/high |
| Peak flow | Low | Low |
| Examples | COPD, asthma | Interstitial lung disease, fibrosis |
Источник: https://www.lecturio.com/magazine/pulmonary-function-tests-pft/
Pulmonary Function Test: Purpose, Procedure & Risks
Pulmonary function tests (PFTs) are a group of tests that measure how well your lungs work. This includes how well you’re able to breathe and how effective your lungs are able to bring oxygen to the rest of your body.
Your doctor may order these tests:
- if you’re having symptoms of lung problems
- if you’re regularly exposed to certain substances in the environment or workplace
- to monitor the course of chronic lung disease, such as asthma or chronic obstructive pulmonary disease (COPD)
- to assess how well your lungs are working before you have surgery
PFTs are also known as lung function tests.
Your doctor will order these tests to determine how your lungs are working. If you already have a condition that’s affecting your lungs, your doctor may order this test to see if the condition is progressing or how it’s responding to treatment.
PFTs can help diagnose:
- asthma
- allergies
- chronic bronchitis
- respiratory infections
- lung fibrosis
- bronchiectasis, a condition in which the airways in the lungs stretch and widen
- COPD, which used to be called emphysema
- asbestosis, a condition caused by exposure to asbestos
- sarcoidosis, an inflammation of your lungs, liver, lymph nodes, eyes, skin, or other tissues
- scleroderma, a disease that affects your connective tissue
- pulmonary tumor
- lung cancer
- weaknesses of the chest wall muscles
If you’re on medications that open your airways, such as those used for asthma or chronic bronchitis, your doctor may ask you to stop taking them before the test.
If it isn’t clear whether or not you should take your medication, make sure to ask your doctor. Pain medications may also affect the results of the test.
You should tell your doctor about any over-the-counter and prescription pain medications you’re taking.
[attention type=yellow][attention type=green][attention type=red]It’s important that you don’t eat a large meal before testing. A full stomach can prevent your lungs from inhaling fully.
[/attention][/attention][/attention]
You should also avoid food and drinks that contain caffeine, such as chocolate, coffee, and tea, before your test. Caffeine can cause your airways to be more open which could affect the results of your test.
You should also avoid smoking at least an hour before the test, as well as strenuous exercise before the test.
Be sure to wear loose-fitting clothing to the test. Tighter clothing may restrict your breathing. You should also avoid wearing jewelry that might affect your breathing. If you wear dentures, wear them to the test to ensure that your mouth can fit tightly around the mouthpiece used for the test.
If you have had recent eye, chest, or abdominal surgery or a recent heart attack, you will ly need to delay the test until you have fully recovered.
Your PFTs may include spirometry, which measures the amount of air you breathe in and out. For this test, you’ll sit in front of a machine and be fitted with a mouthpiece.
It’s important that the mouthpiece fits snugly so that all the air you breathe goes into the machine. You’ll also wear a nose clip to keep you from breathing air out through your nose.
The respiratory technologist will explain how to breathe for the test.
You may then breathe normally. Your doctor will ask you to breathe in and out as deeply or as quickly as you can for several seconds. They may also ask you to breathe in a medication that opens your airways. You’ll then breathe into the machine again to see if the medication affected your lung function.
Plethysmography test
A plethysmography test measures the volume of gas in your lungs, known as lung volume. For this test, you’ll sit or stand in a small booth and breathe into a mouthpiece. Your doctor can learn about your lung volume by measuring the pressure in the booth.
Diffusion capacity test
This test evaluates how well the small air sacks inside the lungs, called alveoli, work. For this part of a pulmonary function test, you will be asked to breathe in certain gases such as oxygen, helium, or carbon dioxide.
You may also breathe in a “tracer gas” for one breath. The machine can detect when you breathe out this gas. This tests how well your lungs are able to transfer oxygen and carbon dioxide to and from your bloodstream.
A PFT can cause problems if:
- you’ve recently had a heart attack
- you’ve recently had eye surgery
- you’ve recently had chest surgery
- you’ve recently had abdominal surgery
- you have a severe respiratory infection
- you have unstable heart disease
PFTs are usually safe for most people. However, because the test may require you to breathe in and out quickly, you may feel dizzy and there’s a risk that you may faint. If you feel lightheaded, tell your doctor. If you have asthma, the test may cause you to have an asthma attack. In very rare cases, PFTs may cause a collapsed lung.
Источник: https://www.healthline.com/health/pulmonary-function-tests
Pulmonary Function Tests
Linkedin Pinterest
Pulmonary function tests (PFTs) are noninvasive tests that show how wellthe lungs are working. The tests measure lung volume, capacity, rates offlow, and gas exchange. This information can help your healthcare providerdiagnose and decide the treatment of certain lung disorders.
There are 2 types of disorders that cause problems with air moving in and the lungs:
- Obstructive. This is when air has trouble flowing the lungs due to airway resistance. This causes a decreased flow of air.
- Restrictive. This is when the lung tissue and/or chest muscles can’t expand enough. This creates problems with air flow, mostly due to lower lung volumes.
PFT can be done with 2 methods. These 2 methods may be used together andperform different tests, depending on the information that your healthcareprovider is looking for:
- Spirometry. A spirometer is a device with a mouthpiece hooked up to a small electronic machine.
- Plethysmography. You sit or stand inside an air-tight box that looks a short, square telephone booth to do the tests.
PFT measures:
- Tidal volume (VT). This is the amount of air inhaled or exhaled during normal breathing.
- Minute volume (MV). This is the total amount of air exhaled per minute.
- Vital capacity (VC). This is the total volume of air that can be exhaled after inhaling as much as you can.
- Functional residual capacity (FRC). This is the amount of air left in lungs after exhaling normally.
- Residual volume. This is the amount of air left in the lungs after exhaling as much as you can.
- Total lung capacity. This is the total volume of the lungs when filled with as much air as possible.
- Forced vital capacity (FVC). This is the amount of air exhaled forcefully and quickly after inhaling as much as you can.
- Forced expiratory volume (FEV). This is the amount of air expired during the first, second, and third seconds of the FVC test.
- Forced expiratory flow (FEF). This is the average rate of flow during the middle half of the FVC test.
- Peak expiratory flow rate (PEFR). This is the fastest rate that you can force air your lungs.
Normal values for PFTs vary from person to person. The amount of airinhaled and exhaled in your test results are compared to the average forsomeone of the same age, height, sex, and race. Results are also comparedto any of your previous test results. If you have abnormal PFT measurementsor if your results have changed, you may need other tests.
Why might I need pulmonary function tests?
There are many different reasons why pulmonary function tests (PFTs) may bedone. They are sometimes done in healthy people as part of a routinephysical.
They are also routinely done in certain types of workenvironments to ensure employee health (such as graphite factories and coalmines).
Or you may have PFTs if your healthcare provider needs help todiagnose you with a health problem such as:
- Allergies
- Respiratory infections
- Trouble breathing from injury to the chest or a recent surgery
- Chronic lung conditions, such as asthma, bronchiectasis, emphysema, or chronic bronchitis
- Asbestosis, a lung disease caused by inhaling asbestos fibers
- Restrictive airway problems from scoliosis, tumors, or inflammation or scarring of the lungs
- Sarcoidosis, a disease that causes lumps of inflammatory cells around organs, such as the liver, lungs, and spleen
- Scleroderma, a disease that causes thickening and hardening of connective tissue
PFTs may be used to check lung function before surgery or other proceduresin patients who have lung or heart problems, who are smokers, or who haveother health conditions. Another use of PFTs is to assess treatment forasthma, emphysema, and other chronic lung problems. Your healthcareprovider may also have other reasons to advise PFTs.
What are the risks of pulmonary function tests?
Because pulmonary function testing is not an invasive procedure, it is safeand quick for most people. But the person must be able to follow clear,simple directions.
All procedures have some risks. The risks of this procedure may include:
- Dizziness during the tests
- Feeling short of breath
- Coughing
- Asthma attack brought on by deep inhalation
In some cases, a person shouldn’t have PFTs. Reasons for this can include:
- Recent eye surgery, because of increased pressure inside the eyes during the procedure
- Recent belly or chest surgery
- Chest pain, recent heart attack, or an unstable heart condition
- A bulging blood vessel (aneurysm) in the chest, belly, or brain
- Active tuberculosis (TB) or respiratory infection, such as a cold or the flu
Your risks may vary depending on your general health and other factors. Askyour healthcare provider which risks apply most to you. Talk with him orher about any concerns you have.
Certain things can make PFTs less accurate. These include:
- The degree of patient cooperation and effort
- Use of medicines that open the airways (bronchodilators)
- Use of pain medicines
- Pregnancy
- Stomach bloating that affects the ability to take deep breaths
- Extreme tiredness or other conditions that affect a person’s ability to do the tests (such as a head cold)
How do I get ready for pulmonary function tests?
Your healthcare provider will explain the procedure to you. Ask him or herany questions you have. You may be asked to sign a consent form that givespermission to do the procedure. Read the form carefully. Ask questions ifanything is not clear.
Tell your healthcare provider if you take any medicines. This includesprescriptions, over-the-counter medicines, vitamins, and herbalsupplements.
Make sure to:
- Stop taking certain medicines before the procedure, if instructed by your healthcare provider
- Stop smoking before the test, if instructed by your healthcare provider. Ask your provider how many hours before the test you should stop smoking.
- Not eat a heavy meal before the test, if instructed by your healthcare provider
- Follow any other instructions your healthcare provider gives you
Your height and weight will be recorded before the test. This is done sothat your results can be accurately calculated.
What happens during pulmonary function tests?
You may have your procedure as an outpatient. This means you go home thesame day. Or it may be done as part of a longer stay in the hospital. Theway the procedure is done may vary. It depends on your condition and yourhealthcare provider's methods. In most cases, the procedure will followthis process:
You’ll be asked to loosen tight clothing, jewelry, or other things that may cause a problem with the procedure.
If you wear dentures, you will need to wear them during the procedure.
You’ll need to empty your bladder before the procedure.
You’ll sit in a chair. A soft clip will be put on your nose. This is so all of your breathing is done through your mouth, not your nose.
You’ll be given a sterile mouthpiece that is attached to a spirometer.
You’ll form a tight seal over the mouthpiece with your mouth. You’ll be instructed to inhale and exhale in different ways.
You will be watched carefully during the procedure for dizziness, trouble breathing, or other problems.
You may be given a bronchodilator after certain tests. The tests will then be repeated several minutes later, after the bronchodilator has taken effect.
What happens after pulmonary function tests?
If you have a history of lung or breathing problems, you may be tired afterthe tests. You will be given a chance to rest afterwards. Your healthcareprovider will talk with you about your test results.
Источник: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pulmonary-function-tests
Pulmonary Function Tests: Categories & Calculations
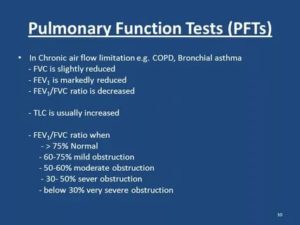
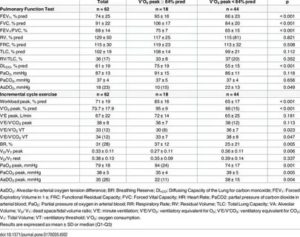
Image: Doing a spirometry, by Jmarchn. License: CC BY-SA 3.0
PFT (pulmonary function tests) can measure lung mechanics (spirometry and lung volumes) or the gas exchange/diffusion function of the respiratory system.
Categories of PFT
There are 3 categories of tests:
Spirometry: FVC and FEV1
- Measures volume of air exhaled as a function of time
- Restrictive lung disease has a reduced volume, i.e. a low FVC
- Obstructive lung disease has a reduced flow, i.e. a low FEV1
Lung volumes: TLC, RV
- The addition of 2 or more volumes comprises a capacity
- Nitrogen washout and helium dilution technique
- Body plethysmography is the standard for measuring lung volumes
Image: Body box with male subject enclosed, by Finchbook01. License: CC BY-SA 3.0
Gas Exchange: DLCO, AaDO2
- Ability to transport gas from alveoli to blood
- Estimates surface area available for gas exchange
- Depends on hemoglobin (Hb) and cardiac output
Indication of PFT
Pulmonary function tests (PFT) are mainly diagnostic/prognostic.
- Diagnostic: screening of at-risk patients, such as age > 70 years, obese; evaluation of chronic cough; follow-up for patients with chronic lung disease
- Prognostic: before lung surgery, to evaluate response to drugs, and to assess the degree of disability
Contraindications of PFT
Recent eye surgery, abdominal aneurysms, hemoptysis, pneumothorax, and recent myocardial infarction.
Lung Volumes and Capacities
Volumes
Tidal volume (TV or VT): volume of air inhaled or exhaled during regular respiration at rest; normal value: 500 ml
Inspiratory reserve volume (IRV): volume of air that can be maximally inhaled above and after a normal tidal inspiration; normal value: 3,000 ml
Expiratory reserve volume (ERV): volume of air that can be maximally exhaled after a normal tidal expiration; normal value: 1,500 ml
Residual volume (RV): the amount of air that remains in the lungs after maximal forced exhalation; cannot be measured directly by spirometry but is indirectly calculated as RV = FRC – ERV; normal value: 20–25mL/kg or 1,200 mL.
Capacities (sum of 2 or more volumes)
Total lung capacity (TLC): volume of air present in lungs after maximum deep inspiration; the sum of all volumes: TLC = IRV + TV + ERV + RV; normal value: 5,000–6,000 ml
Vital capacity (VC): maximum volume of air exhaled after a maximum deep inspiration: VC = IRV + TV + ERV or VC = TLC – RV; normal value: 4,500–5,000 ml
Inspiratory capacity (IC): maximum volume of air inspired after a normal tidal expiration: IC = TV + IRV; normal value: 2,400–3,600 ml
Expiratory capacity (EC): maximum volume of air expired after normal tidal inspiration: EC = TV+ ERV; normal value: 1,800–2,300 ml
Functional residual capacity (FRC): volume of air remaining in the lungs after normal tidal expiration: FRC = ERV + RV.
FRC is an important component that maintains a continuous exchange of oxygen and carbon dioxide at the alveolar-capillary membrane.
Collapse or atelectasis of the lungs leads to a reduction in FRC, causing hypoxemia and hypercarbia. The normal value is 2,500 ml.
Image: Functional residual capacity
Spirometry
Image: Doing a spirometry, by Jmarchn. License: CC BY-SA 3.0
Spirometry is the most frequently used measure of pulmonary function. It measures the volume of air inhaled or exhaled by the patient as a function of time. The patient is asked to take a deep inspiration and then to forcefully expel air, as quickly and as long as possible. The results of the test include:
- Forced vital capacity (FVC): maximum volume of air forcefully exhaled after a maximal inspiration. This is usually reduced in restrictive lung disease; however, an obstructive lung disease with significant hyperinflation can also cause reduced FVC.
- FEV1: volume of air exhaled during the initial second of the FVC maneuver.
- The ratio of FEV1/FVC: Normal value is > 75%. The value is decreased in obstructive lung disease. Values < 50% suggests a severe obstruction.
- FEF 25–75% (forced mid-expiratory flow): maximum flow rate during mid-expiratory part of the FVC maneuver. Expressed in L/min, it represents the status of small airways. Normal value is 300 L/min.
- PEFR (peak expiratory flow rate): Maximal flow rate during the FVC maneuver occurs in the initial 0.1 seconds. It gives a crude estimate of larger airway function. Normal value is 400–700 L/min.
Important: Spirometry does not measure volumes such as FRC, TC, and RV.
Two patterns of results are identified: obstructive and restrictive diseases.
In obstructive diseases, a reduction in flow is predominant, leading to low FEV1; however, FVC may be normal or low. Hence, the FEV1/FVC ratio is usually < 0.7.
Reversibility: An increase in FEV1 by 12–15% on repeat spirometry after administration of a bronchodilator (salbutamol) is characteristic of asthma.
[attention type=green][attention type=red][attention type=yellow]In restrictive diseases, a reduction in lung volume is predominant, which leads to low FVC; however, FEV1 may be normal or low. Hence, FEV1/FVC ratio is > 0.7 (and may be > 1.0).
[/attention][/attention][/attention]
This needs confirmation, as RV cannot be measured by spirometry (low RV is the hallmark of restrictive lung disease).
Loop spirometry
Image: Loop spirometry
Flow volume loops are formed when a patient performs the spirometry maneuver, and a graph is plotted with the volume on the x-axis and the flow on the y-axis. The expiratory limb is usually represented as positive.
The initial one-third of the expiratory flow is effort dependant; the latter part is effort independent; hence the shape.
The inspiratory limb is entirely effort dependent, and the curve is smooth (useful for identifying the phase of respiration if not labeled).
In the obstructive pattern of the flow-volume loop, there is a decrease in the height of the y-axis, which represents decreased air flow. The volume remains normal or high (hyper-inflation). In the restrictive pattern, there is predominantly reduced volume, which is more prominent than the decrease in flow.
Image: Loop spirometry
Limitation of spirometry
Spirometry cannot measure RV or TLC. It is important to differentiate the cause of decreased VC in a patient suffering from chronic obstructive pulmonary disease (COPD). In COPD, VC can be reduced in two scenarios:
- The patient has a superimposed restrictive lung disease.
- The patient has significant hyper-inflation.
These can be differentiated using lung volume measurement. The former will have a reduced TLC, while hyper-inflation will show increased TLC. Hence, a confirmation by lung volume studies is necessary.
Detection of upper airway obstruction–other spirometry patterns
Image: Detection of upper airway obstruction
- Fixed airway obstruction: constant limitation of flow during inspiration and expiration; for example: stricture, goiter, or stenosis
- Variable extrathoracic obstruction: Reduction in flow is greater during inspiration (airways tend to collapse during inspiration due to negative transmural pressure). Positive pressure in airway during expiration decreases obstruction. For example: vocal cord palsy, obstructive sleep apnea
- Variable intrathoracic obstruction: Reduction inflow is greater during expiration (high pleural pressure decreases airway diameter). During inspiration, lower pleural pressure around the airway tends to decrease obstruction. For example: tracheomalacia, tumor of bronchus
Lung Volumes – RV, FRC, TLC
Gas dilution technique
N2 washout: Patient breathes 100% oxygen, so that all nitrogen in the lungs is washed out. The difference in nitrogen volume at initial exhaled concentration and final concentration gives the value of FRC.
He dilution: Patient breathes from a reservoir containing a known volume of gas with a trace of helium. The inhaled helium gets diluted in the gas present in lungs.
The concentration of helium in the exhaled gas is expressed as a percentage, giving the lung volume.
For example, if the patient breathes 50 mL of helium, and its concentration in the exhaled gas is 1%, the volume of the lung is 5 L.
Plethysmography
The patient sits inside an airtight body box with a known volume. The patient pants with an open glottis against a closed shutter. The increase in chest volume reduces the relative box volume and increases the box pressure. Measurements are done during expiration, and hence FRC is measured. The principal behind plethysmography is Boyle’s law (P x V = K).
Important: Lung volumes, such as RV, FRC, and TLC, cannot be measured by spirometry.
Applications of volume testing
- Measures RV, FRC, and TLC (which spirometry cannot measure)
- Spirometry only measures FVC, which can be misleading when used alone.
- Reduced RV, FRC, and TLC is seen in restrictive diseases interstitial lung disease, sarcoidosis, or fibrosis.
- Increased RV, FRC, and TLC is seen in obstructive lung diseases asthma, COPD, and cystic fibrosis.
Gas Exchange Function – DLCO, AaDO2
DLCO (Diffusion capacity of Carbon Monoxide)
The patient inspires a diluted mixture of CO and is told to hold their breath for 10 seconds. The amount of CO taken up is then measured by infrared analysis.
DLCO = CO (ml/min/mm Hg) ÷ PACO – PcCO
CO is the ideal gas for this study, as it has a very high affinity for Hb and very low plasma/lung concentration. It demonstrates the ability of the lung to transport inhaled gas from the alveoli to the blood. Normal value is 20–30 ml/min/mm Hg.
DLCO values depend on three factors:
- Thickness and permeability of alveolar-capillary membrane (increased in pulmonary bleeding, interstitial lung disease)
- Hemoglobin concentration
- Cardiac output
Factors altering DLCO
| Decrease DLCO (< 80%) | Increase DLCO (> 120%) |
| Anemia | Polycythemia |
| Emphysema | Exercise |
| Fibrosis | Congestive heart failure |
Alveolar to arterial oxygen tension gradient (AaDO2)
- Detects the difference between alveolar oxygen (PaO2) and arterial oxygen tension (PaO2)
- Needs arterial blood gas analysis for PaO2
- Normal values are below 10 mm Hg, and values above 100 mm Hg indicate significant impairment in gas exchange.
Cardiopulmonary reserve/exercise testing
- The stair-climbing test and 6-minute walk test measure changes in SaO2/SpO2, HR, and oxygen utilization (VaO2).
- These tests analyze the individual’s ability to cope with increased metabolic demands during exercise.
- They give a clear picture of the functional improvement of a patient during follow-up.
Summary
| Parameter | Obstructive lung disease | Restrictive lung disease |
| TLC | High/normal | Very low |
| VC or FVC | Low/normal | Very low |
| RV | High | Low |
| FRC | High | Low |
| FEV1 | Very Low | Normal/low |
| FEV1/FVC | Low | Normal/high |
| Peak flow | Low | Low |
| Examples | COPD, asthma | Interstitial lung disease, fibrosis |
Источник: https://www.lecturio.com/magazine/pulmonary-function-tests-pft/
Pulmonary Function Test: Purpose, Procedure & Risks
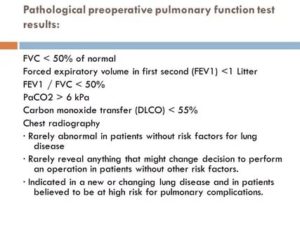
Pulmonary function tests (PFTs) are a group of tests that measure how well your lungs work. This includes how well you’re able to breathe and how effective your lungs are able to bring oxygen to the rest of your body.
Your doctor may order these tests:
- if you’re having symptoms of lung problems
- if you’re regularly exposed to certain substances in the environment or workplace
- to monitor the course of chronic lung disease, such as asthma or chronic obstructive pulmonary disease (COPD)
- to assess how well your lungs are working before you have surgery
PFTs are also known as lung function tests.
Your doctor will order these tests to determine how your lungs are working. If you already have a condition that’s affecting your lungs, your doctor may order this test to see if the condition is progressing or how it’s responding to treatment.
PFTs can help diagnose:
- asthma
- allergies
- chronic bronchitis
- respiratory infections
- lung fibrosis
- bronchiectasis, a condition in which the airways in the lungs stretch and widen
- COPD, which used to be called emphysema
- asbestosis, a condition caused by exposure to asbestos
- sarcoidosis, an inflammation of your lungs, liver, lymph nodes, eyes, skin, or other tissues
- scleroderma, a disease that affects your connective tissue
- pulmonary tumor
- lung cancer
- weaknesses of the chest wall muscles
If you’re on medications that open your airways, such as those used for asthma or chronic bronchitis, your doctor may ask you to stop taking them before the test.
If it isn’t clear whether or not you should take your medication, make sure to ask your doctor. Pain medications may also affect the results of the test.
You should tell your doctor about any over-the-counter and prescription pain medications you’re taking.
[attention type=yellow][attention type=green][attention type=red]It’s important that you don’t eat a large meal before testing. A full stomach can prevent your lungs from inhaling fully.
[/attention][/attention][/attention]
You should also avoid food and drinks that contain caffeine, such as chocolate, coffee, and tea, before your test. Caffeine can cause your airways to be more open which could affect the results of your test.
You should also avoid smoking at least an hour before the test, as well as strenuous exercise before the test.
Be sure to wear loose-fitting clothing to the test. Tighter clothing may restrict your breathing. You should also avoid wearing jewelry that might affect your breathing. If you wear dentures, wear them to the test to ensure that your mouth can fit tightly around the mouthpiece used for the test.
If you have had recent eye, chest, or abdominal surgery or a recent heart attack, you will ly need to delay the test until you have fully recovered.
Your PFTs may include spirometry, which measures the amount of air you breathe in and out. For this test, you’ll sit in front of a machine and be fitted with a mouthpiece.
It’s important that the mouthpiece fits snugly so that all the air you breathe goes into the machine. You’ll also wear a nose clip to keep you from breathing air out through your nose.
The respiratory technologist will explain how to breathe for the test.
You may then breathe normally. Your doctor will ask you to breathe in and out as deeply or as quickly as you can for several seconds. They may also ask you to breathe in a medication that opens your airways. You’ll then breathe into the machine again to see if the medication affected your lung function.
Plethysmography test
A plethysmography test measures the volume of gas in your lungs, known as lung volume. For this test, you’ll sit or stand in a small booth and breathe into a mouthpiece. Your doctor can learn about your lung volume by measuring the pressure in the booth.
Diffusion capacity test
This test evaluates how well the small air sacks inside the lungs, called alveoli, work. For this part of a pulmonary function test, you will be asked to breathe in certain gases such as oxygen, helium, or carbon dioxide.
You may also breathe in a “tracer gas” for one breath. The machine can detect when you breathe out this gas. This tests how well your lungs are able to transfer oxygen and carbon dioxide to and from your bloodstream.
A PFT can cause problems if:
- you’ve recently had a heart attack
- you’ve recently had eye surgery
- you’ve recently had chest surgery
- you’ve recently had abdominal surgery
- you have a severe respiratory infection
- you have unstable heart disease
PFTs are usually safe for most people. However, because the test may require you to breathe in and out quickly, you may feel dizzy and there’s a risk that you may faint. If you feel lightheaded, tell your doctor. If you have asthma, the test may cause you to have an asthma attack. In very rare cases, PFTs may cause a collapsed lung.
Источник: https://www.healthline.com/health/pulmonary-function-tests
Pulmonary Function Tests
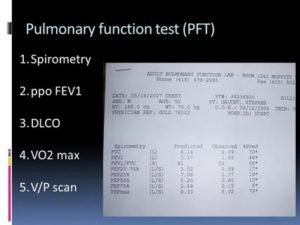
Linkedin Pinterest
Pulmonary function tests (PFTs) are noninvasive tests that show how wellthe lungs are working. The tests measure lung volume, capacity, rates offlow, and gas exchange. This information can help your healthcare providerdiagnose and decide the treatment of certain lung disorders.
There are 2 types of disorders that cause problems with air moving in and the lungs:
- Obstructive. This is when air has trouble flowing the lungs due to airway resistance. This causes a decreased flow of air.
- Restrictive. This is when the lung tissue and/or chest muscles can’t expand enough. This creates problems with air flow, mostly due to lower lung volumes.
PFT can be done with 2 methods. These 2 methods may be used together andperform different tests, depending on the information that your healthcareprovider is looking for:
- Spirometry. A spirometer is a device with a mouthpiece hooked up to a small electronic machine.
- Plethysmography. You sit or stand inside an air-tight box that looks a short, square telephone booth to do the tests.
PFT measures:
- Tidal volume (VT). This is the amount of air inhaled or exhaled during normal breathing.
- Minute volume (MV). This is the total amount of air exhaled per minute.
- Vital capacity (VC). This is the total volume of air that can be exhaled after inhaling as much as you can.
- Functional residual capacity (FRC). This is the amount of air left in lungs after exhaling normally.
- Residual volume. This is the amount of air left in the lungs after exhaling as much as you can.
- Total lung capacity. This is the total volume of the lungs when filled with as much air as possible.
- Forced vital capacity (FVC). This is the amount of air exhaled forcefully and quickly after inhaling as much as you can.
- Forced expiratory volume (FEV). This is the amount of air expired during the first, second, and third seconds of the FVC test.
- Forced expiratory flow (FEF). This is the average rate of flow during the middle half of the FVC test.
- Peak expiratory flow rate (PEFR). This is the fastest rate that you can force air your lungs.
Normal values for PFTs vary from person to person. The amount of airinhaled and exhaled in your test results are compared to the average forsomeone of the same age, height, sex, and race. Results are also comparedto any of your previous test results. If you have abnormal PFT measurementsor if your results have changed, you may need other tests.
Why might I need pulmonary function tests?
There are many different reasons why pulmonary function tests (PFTs) may bedone. They are sometimes done in healthy people as part of a routinephysical.
They are also routinely done in certain types of workenvironments to ensure employee health (such as graphite factories and coalmines).
Or you may have PFTs if your healthcare provider needs help todiagnose you with a health problem such as:
- Allergies
- Respiratory infections
- Trouble breathing from injury to the chest or a recent surgery
- Chronic lung conditions, such as asthma, bronchiectasis, emphysema, or chronic bronchitis
- Asbestosis, a lung disease caused by inhaling asbestos fibers
- Restrictive airway problems from scoliosis, tumors, or inflammation or scarring of the lungs
- Sarcoidosis, a disease that causes lumps of inflammatory cells around organs, such as the liver, lungs, and spleen
- Scleroderma, a disease that causes thickening and hardening of connective tissue
PFTs may be used to check lung function before surgery or other proceduresin patients who have lung or heart problems, who are smokers, or who haveother health conditions. Another use of PFTs is to assess treatment forasthma, emphysema, and other chronic lung problems. Your healthcareprovider may also have other reasons to advise PFTs.
What are the risks of pulmonary function tests?
Because pulmonary function testing is not an invasive procedure, it is safeand quick for most people. But the person must be able to follow clear,simple directions.
All procedures have some risks. The risks of this procedure may include:
- Dizziness during the tests
- Feeling short of breath
- Coughing
- Asthma attack brought on by deep inhalation
In some cases, a person shouldn’t have PFTs. Reasons for this can include:
- Recent eye surgery, because of increased pressure inside the eyes during the procedure
- Recent belly or chest surgery
- Chest pain, recent heart attack, or an unstable heart condition
- A bulging blood vessel (aneurysm) in the chest, belly, or brain
- Active tuberculosis (TB) or respiratory infection, such as a cold or the flu
Your risks may vary depending on your general health and other factors. Askyour healthcare provider which risks apply most to you. Talk with him orher about any concerns you have.
Certain things can make PFTs less accurate. These include:
- The degree of patient cooperation and effort
- Use of medicines that open the airways (bronchodilators)
- Use of pain medicines
- Pregnancy
- Stomach bloating that affects the ability to take deep breaths
- Extreme tiredness or other conditions that affect a person’s ability to do the tests (such as a head cold)
How do I get ready for pulmonary function tests?
Your healthcare provider will explain the procedure to you. Ask him or herany questions you have. You may be asked to sign a consent form that givespermission to do the procedure. Read the form carefully. Ask questions ifanything is not clear.
Tell your healthcare provider if you take any medicines. This includesprescriptions, over-the-counter medicines, vitamins, and herbalsupplements.
Make sure to:
- Stop taking certain medicines before the procedure, if instructed by your healthcare provider
- Stop smoking before the test, if instructed by your healthcare provider. Ask your provider how many hours before the test you should stop smoking.
- Not eat a heavy meal before the test, if instructed by your healthcare provider
- Follow any other instructions your healthcare provider gives you
Your height and weight will be recorded before the test. This is done sothat your results can be accurately calculated.
What happens during pulmonary function tests?
You may have your procedure as an outpatient. This means you go home thesame day. Or it may be done as part of a longer stay in the hospital. Theway the procedure is done may vary. It depends on your condition and yourhealthcare provider's methods. In most cases, the procedure will followthis process:
You’ll be asked to loosen tight clothing, jewelry, or other things that may cause a problem with the procedure.
If you wear dentures, you will need to wear them during the procedure.
You’ll need to empty your bladder before the procedure.
You’ll sit in a chair. A soft clip will be put on your nose. This is so all of your breathing is done through your mouth, not your nose.
You’ll be given a sterile mouthpiece that is attached to a spirometer.
You’ll form a tight seal over the mouthpiece with your mouth. You’ll be instructed to inhale and exhale in different ways.
You will be watched carefully during the procedure for dizziness, trouble breathing, or other problems.
You may be given a bronchodilator after certain tests. The tests will then be repeated several minutes later, after the bronchodilator has taken effect.
What happens after pulmonary function tests?
If you have a history of lung or breathing problems, you may be tired afterthe tests. You will be given a chance to rest afterwards. Your healthcareprovider will talk with you about your test results.
Источник: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pulmonary-function-tests
Источник: https://ru.medic-life.com/pulmonary-function-test-8828
